Guest contribution:
 Article series on the subject of state-of-the-art mycology in dermatology,
Article series on the subject of state-of-the-art mycology in dermatology,
11th article
by Prof Hans-Jürgen Tietz, Director of the Institute of Fungal Diseases in Berlin, Germany
Fungal cultures and their aesthetically pleasing structures will always hold a special place in my heart, but even I must admit that the introduction of PCR into mycological diagnostics was revolutionary. I have been even more impressed and convinced in recent years by the possibilities of gene-based mycological diagnostics for both diagnosis and therapy.
A current example:

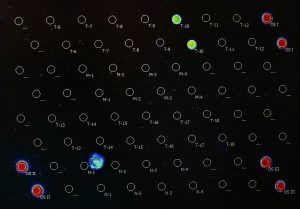
A 3-year-old boy with Tinea corporis after the purchase of three guinea pigs, who presented due to increasing generalisation with local therapy (Fig. 1a). Samples were taken using a DNA-free sampling swab and the results by PCR diagnostics came back less than 48 hours later: T. benhamiae (Fig. 1b). Additional systemic therapy with SUBA®-itraconazole, administered in mashed banana, could be started immediately.
This is faster and more precise than in any other discipline of infectiology and represents a major shift in mycology. It now stands on an equal footing with virology – the only difference being that we can heal any infection.
A similar case led me on my own road to Damascus three years ago and my colleagues and I introduced PCR diagnostics for mycoses into our practice laboratory as an addition to diagnostics by culture. Since then, many doctors in private practice have followed suit, while some pioneers had introduced it even earlier. But what is the situation at dermatology clinics, considering the threat posed by new fungal pathogens from all over the world?
There are T. benhamiae from Japan, T. mentagrophytes type VII from Thailand, T. mentagrophytes type VIII (new name: T. indotineae), a novel, highly terbafine-resistent species from India (1), T. erinacei, M. audouinii, T. violaceum, T. soudanense, T. tonsurans and T. schoenleinii, that have often reached us from Africa, as well as T. quinckeanum, a novel domestic pathogen that continues to emerge more frequently.
On the premises of the Department of Dermatology of the Charité, where the causative agent of syphilis as well as T. interdigitale, A. gertleri and C. africana were discovered, now stands a world-renowned institute of virology. And regarding COVID-19, the overarching Humboldt University is bustling with doctors, modellers and epidemiologists, who appear in prime-time talks with TV presenter Markus Lanz. What is the position of mycology here? The department of dermatology established PCR in mycology a long time ago and would deserve an academic chair for infectious diseases with focus on mycology. But many dermatological departments no longer even have mycology laboratories or they were moved to microbiology.
Our clinics are beacons for this medical field and they are where new mycologists are educated. Mycology is still enshrined in residency as an indispensable foundation of dermatology – thank goodness. But that also means the following: No dermatology clinic without a mycology laboratory. No teaching hospital without PCR – an absolute necessity for the benefit of the patient and the given right to advanced training, which should be an obligation for as long as it exists.
Prospects: Mycology laboratories and PCR should be part of every clinic and should be priced into the budget. Many practice laboratories have succeeded in doing so and are excited about the new possibilities for diagnosis. Clinics must now follow suit – so there is a lot to be done. May it be a successful new year in this regard.
Sincerely yours,
Hans-Jürgen Tietz
The articles under the rubric “Guest contribution” only reflect the views of the respective authors. Responsibility for the legality and content of the articles lies solely with the authors. EUROIMMUN does not assume liability for the completeness, accuracy and currentness of the information provided.

