Bone metabolic diseases are a major health problem, causing bone fractures, skeletal pain and deformities.
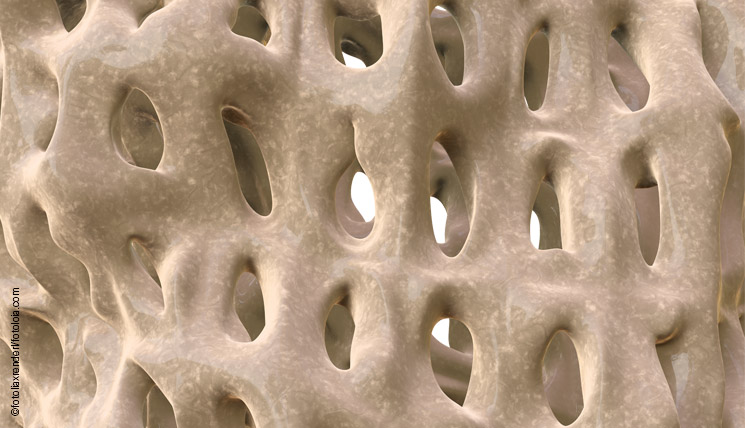
Bone tissue is a living tissue which is composed of cells (osteocytes) and a mineral extracellular matrix. This comprises mostly calcium phosphate in crystalline form (hydroxyapatite) that is incorporated into an organic protein matrix consisting largely of type I collagen. While the hydroxyapatite is responsible for the rigidity of the skeleton, the collagen fibrils provide bone with its elasticity. On the cellular level, bone tissue can be divided into two main cell types which work closely together to regulate the continuous, dynamic bone remodelling: osteoblasts are bone-producing cells which synthesise the proteins necessary for building the extracellular matrix. Osteoclasts on the other hand function osteolytically, releasing protons and proteases responsible for the degradation of bone material. Both types of cells and therewith the calcium metabolism are regulated by hormones, growth factors and cytokines. The three main regulators are parathyroid hormone (PTH), calcitonin and vitamin D.
PTH is synthesised in the parathyroid glands and released as soon as the calcium level in the blood is low. Intact PTH (iPTH), the biologically active form, indirectly stimulates the formation of osteoclasts, which increases bone resorption and release of calcium.
Calcitonin (thyrocalcitonin, human calcitonin, HCT) is produced in the thyroid gland and is the antagonist of PTH. The production and secretion of calcitonin is stimulated by an elevated calcium level. It increases mineralisation and synthesis of bone matrix leading to a reduction in the calcium concentration in the blood.
Vitamin D is produced in skin exposed to ultraviolet B radiation and acquired by consumption of certain foods. In the kidneys the vitamin becomes the biologically active metabolite 1,25-dihydroxy vitamin D that regulates calcium uptake from the intestine and bone mineralisation.
Imbalances in bone metabolism
Dysregulation of this complex regulation network, e. g. in form of hyper- or hypothyroidism or hypovitaminosis D, can have different reasons and may cause serious long-term consequences.
An uncontrolled increase in the level of PTH results in hyperthyroidism (HPT). It may be due to a parathyroid gland adenoma or rarely a carcinoma (primary HPT) or a reactive increase in PTH as a result of hypocalcaemia caused by kidney, liver or intestinal disease (secondary HPT). Consequences of HPT may be specific bone changes with a reduction in bone mass (osteopenia or osteoporosis) or kidney stones.
A deficiency in PTH results in hypoparathyroidism. This usually occurs following a throat operation. It is generally iatrogenic, e.g. due to inadvertent removal of parathyroid glands during thyroidectomy, following radioiodine therapy or in cases of malignant parathyroid gland tumours. Symptoms of hypoparathyroidism are hypocalcaemia with cramps and heart failure.
Vitamin D deficiency, named hypovitaminosis D, is mainly caused by insufficient exposure to UV light and a vitamin D deficient diet. Vitamin D undersupply has manifold health consequences, e. g. a secondary increase in PTH and an elevated osteolysis rate. Severe vitamin D deficiency is also associated with the development of dementia, autoimmune diseases and certain types of cancer.
Diagnostics of bone metabolic diseases
The serological determination of iPTH, calcitonin and vitamin D plays an important role in the diagnosis of bone metabolic diseases and related conditions. It supports other diagnostic methods such as case history, physical examination, radiographic analysis, bone biopsy and other laboratory tests.
iPTH determination using ELISA is an essential component in the diagnosis of functional disorders of the parathyroid gland. It is the most important serological test for the diagnosis of primary HPT, and supports clarification of the different HPT forms.
Calcitonin ELISA, in addition to its application in bone disease diagnostics, is also of major importance for diagnosing and monitoring medullar thyroid carcinoma (C-cell carcinoma). The serum calcitonin level is strongly increased in this type of cancer. After successful total thyroidectomy, calcitonin is no longer detectable. Increasing concentrations of calcitonin after therapy indicate relapse or metastasis.
The serum level of 25-OH vitamin D, which of all vitamin D metabolites in the blood shows the highest and most stable concentration, is the best indicator of the vitamin D supply in the body. Low 25-OH vitamin D concentration measured by ELISA points to an existing undersupply. Regular monitoring of the vitamin D level in patients under treatment is also important to evaluate the individual therapy response.