Uromodulin, which was first described as Tamm-Horsfall protein in 1950, is an important biomarker in nephrology. The protein is exclusively expressed in the kidney and is mostly secreted into the renal tubules. A small amount also ends up in the blood circulation. Both uromodulin concentration in urine as well as in serum are used as indicators for kidney function. However, determination of uromodulin concentration in serum has the advantage that serum uromodulin exists as monomers, compared to the polymerized form found in urine.. Therefore, measuring results in serum exhibit a higher reproducibility [1].
Uromodulin in nephrology
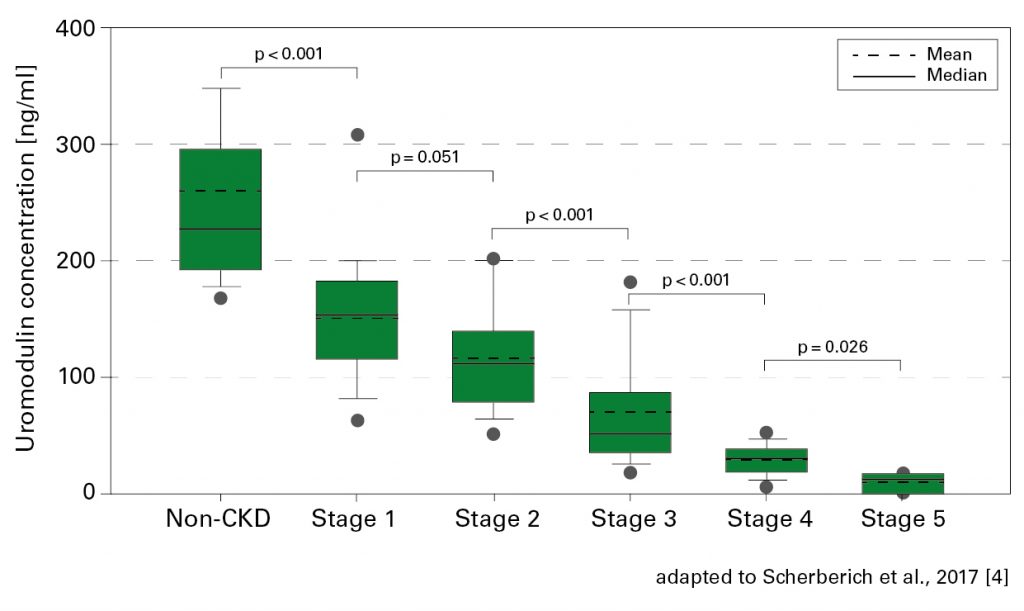 In 2014, Swiss authors reported for the first time that a decrease of uromodulin levels in serum comes along with a significant impairment of kidney function [2]. Subsequent studies confirmed the correlation of serum concentration with the (estimated) glomerular filtration rate (eGFR) and with the stages of chronic kidney disease as defined by KDIGO (Kidney Disease – Improving Global Outcomes) [see figure; 3, 4]. In contrast to traditional kidney function markers such as serum creatinine, cystatin C and eGFR-cystatin C, the serum level of uromodulin already starts to decrease significantly with the onset of kidney impairment (CKD stage 1). Thus, diminishing kidney functionality can be detected from the very beginning.
In 2014, Swiss authors reported for the first time that a decrease of uromodulin levels in serum comes along with a significant impairment of kidney function [2]. Subsequent studies confirmed the correlation of serum concentration with the (estimated) glomerular filtration rate (eGFR) and with the stages of chronic kidney disease as defined by KDIGO (Kidney Disease – Improving Global Outcomes) [see figure; 3, 4]. In contrast to traditional kidney function markers such as serum creatinine, cystatin C and eGFR-cystatin C, the serum level of uromodulin already starts to decrease significantly with the onset of kidney impairment (CKD stage 1). Thus, diminishing kidney functionality can be detected from the very beginning.
Studies published within the last year additionally dealt with the predictive value of serum uromodulin. Leiherer et al. demonstrated with reference to prospectively collected data from 529 coronary patients that low uromodulin levels in serum are associated with an increased risk for future kidney insufficiency. Thisapplies significantly to patients homozygous for a certain polymorphism of the uromodulin-encoding gene UMOD [5]. Another study reported that those patients with chronic kidney insufficiency who exhibited the relatively lowest uromodulin concentrations in serums were the most likely to proceed to end-stage renal disease [6].
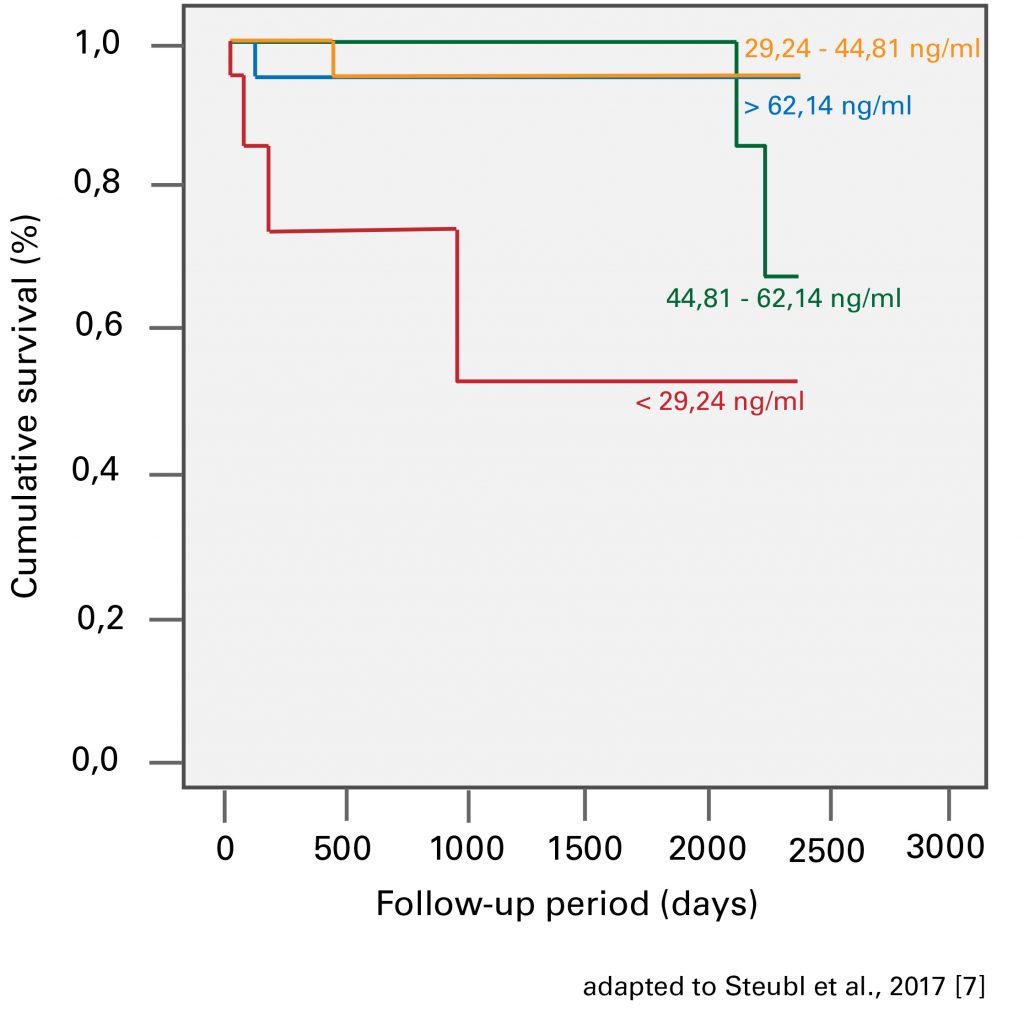 And finally, the team surrounding Prof. Scherberich found out that the chance of graft loss after kidney transplantation will be significantly higher if the serum uromodulin concentration does not rise to a certain threshold within few days after surgery. Thus, the patients with the lowest uromodulin levels were at significantly higher risk for renal transplant failure [see figure; 7].
And finally, the team surrounding Prof. Scherberich found out that the chance of graft loss after kidney transplantation will be significantly higher if the serum uromodulin concentration does not rise to a certain threshold within few days after surgery. Thus, the patients with the lowest uromodulin levels were at significantly higher risk for renal transplant failure [see figure; 7].
New clinical implications of uromodulin
A rapid decrease of kidney function is a risk marker for cardiovascular diseases and overall mortality [8]. In accordance with this, another study from Leiherer et al. showed that determination of serum uromodulin may also be useful to predict cardiovascular events and mortality in coronary patients. This association with uromodulin proved to be independent of glomerular filtration rate and thus, of renal function [9]. Also, in the investigation of more than 3,000 patients referred for coronary angiography, higher serum uromodulin concentrations were associated with a more favorable metabolic profile as well as lower prevalence rates of arterial hypertension, diabetes mellitus, and heart failure [10].
Finally, there are further interesting approaches concerning uromodulin, e.g. a potential role of serum uromodulin as biomarker for diabetes mellitus (type 2) [11] or urinary uromodulin as early indicator of preeclampsia, a severe complication in pregnancy [12]. Therefore, uromodulin will remain an interesting research subject in future years.
[1] Youhanna et al., Nephrol Dial Transplant 0:1-10 (2013) [2] Risch et al., Clin Chem Lab Med 52(12):1755-1761 (2014) [3] Steubl et al., Medicine 95(10):e3011 (2016) [4] Scherberich et al., Nephrol Dial Transplant 1-12 (2017) [5] Leiherer et al., J Hypertension 35:000-000 (2017) [6] Tan et al., Int J Clin Exp Med 10(5):8055-8059 (2017) [7] Steubl et al., Biomarkers 22(2):171-177 (2017) [8] Rein et al., Am J Cardiol 113(2):215-212 (2014) [9] Leiherer et al., Int J Cardiol 231:6-12 (2017) [10] Delgado et al., J Am Soc Nephrol 28(7):2201-2210 (2017) [11] Leiherer et al., Medicine 96:5(e5798) (2017) [12] Kononikhin et al., J Proteomics 149: 38-43 (2016)